Emerging Infectious Diseases and Diagnosis Journal
(ISSN 2652-4449)
Volume 03; Issue 01
Case Report
High Risk of Severe Sars-Cov-2 in Patient with Obesity and Co-morbility: importance of early management from mechanical ventilation to rehabilitation in the Covid-19 Era
Weimer LE1, Cattari G2, Binelli A1, Fanales Belasio E3, Piras S2, Sensi F4
1National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy
2Reparto COVID, Ospedale Marino-Alghero, ASSL Sassari, ATS Sardegna , Italy
3Department of Infectious Diseases , DMI; Istituto Superiore di Sanità, Rome, Italy
4Direzione ASSL Sassari, ATS Sardegna, Italy
*Corresponding author: Liliana Elena Weimer, National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy, Email: liliana.weimer@iss.it
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras , et al. (2021) High Risk of Severe Sars-Cov-2 in Patient with Obe- sity and Co-morbility: importance of early management from mechanical ventilation to rehabilitation in the Covid-19 Era. Emerg Infect Dis Diag J: EIDDJ-100031. DOI: 10.53634/2652-4449.100031
Received date: 17 June, 2021; Accepted date: 02 July 2021; Published date: 09 July, 2021
Abstract
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS Cov2), has resulted in 176 million infections and
3.8 million deaths by 16 June 2021, globally. Obesity, a critical risk factor for respiratory infection, is increasingly being recognized as a predisposing factor in the current coronavirus disease . This has important implications on global health as excess weight, usually represented by a raised body mass index (BMI), affects vast numbers of people worldwide: 39% of adults are overweight (BMI ≥25.0 to 29.9 kg/m2) and 13% have clinical obesity (BMI ≥30.0 kg/m2) globally.
Obesity is associated with increased production of inflammatory cytokines such as TNF-α, interleukins and interferons that characterize chronic low - grade inflammation, which impair immune responses, both innate and adaptive. A hyper inflammatory response in which there are raised levels of interleukins and TNF-α has been associated with increased mortality from COVID-19. The prevalence of obesity in men and women increases with age. We explore in this Case Report the relationship between excess weight and response to infection with SARS-CoV-2, the severity and complications of COVID-19 in a Italian patient with Severe Interstitial Pneumonia and co-morbilities.
Keywords: Obesity; Severe Interstitial Pneumonia; Sars- Cov-2
Description
Our Italian patient 64-year-old , male , developed fever up to 38.7 degrees C, diarrhea, asthenia, myalgia, dyspnea with desaturation and poorly productive cough on 9 April 2021. In the Hospital of Alghero, Sardigna, Italy, he was admitted immediately after computed tomography (CT) imaging of his chest showed multiple and bilateral ground-glass opacities located in both subpleural and apico-basal spaces (especially on the right). Nasopharyngeal swab specimens were collected to detect severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid. The swab specimens were tested by real-time reverse transcriptase–polymerase chain reaction; a positive result was received 1 day later on 10 April 2021.
Our patient was diagnosed with COVID-19 and he received O2 Therapy; methylprednisolone three i.v. boluses of 200mg; Tocilizumab was given in a single i.v. 400-mg dose ; prophylactic enoxaparin 4000 mg x2 was prescribed , prompt protonic inhibitor (pantoprazole 40 mg), diuretic (furosemide 20 mg 1 f), insulin Lantus 4U 22 hours, antihypertensive (amlodipine 5mg, ramipril 5 mg), Pregabalin 150 mg, Trazodone 50 mg three times daily. For Severe Interstitial Pneumonia our patient needed mechanical ventilation and nasal cannulae with and a continuous follow-up of her clinical status.
The patient had a history of arterial hypertension, diabetes mellitus type II, previous Guillain-Barré syndrome, obesity III degree (BMI=40). On day five our patient was sedated with Dexdor (Dexmedetomidine) for poor compliance in holding the continuous positive airway pressure therapy (CPAP) helmet for Severe Pneumonia with (Fi02 50% and P/F 205). On 20 April 2021the sedation was progressively reduced, continuous positive airway pressure therapy (CPAP) ventilation was suspended, and a mask with high-flow reservoir was started ( FiO2 35% pH 7.42, pO2 84 mmHg, pCO2 41 mmHg P/F 240). Biochemistry test indicated leucocytes 9.58 × 10 3c/μl (reference 4-11 × 103c/μl), D-dimer 3.3 μg/ml (reference 0.1-0.5 μg/ml), C-reactiveprotein 329 mg/l (reference 0-5 mg/l), procalcitonin 6.72ng/ml (reference 0-0.1 ng/ml), lactate dehydrogenase 316u/l (reference 135-225 u/l) and lactic acid 3.6 mmol/l (reference 0.5-1 mmol/l).
The response to treatment was refractory. The swab specimens were tested by real-time reverse transcriptase–polymerase chain reaction was positive and our patient continues with a mask with high-flow reservoir (FiO2 35% pH 7.42, pO2 84 mmHg, pCO2 41 mmHg P/F 240). Fortunately, after the maintenance of intensive medical treatment, mechanical ventilation, and Nasal canulae e continuous emogasanalysis in the hospital our patient progressively improved to total recovery.
On May 10, 2021, our patient was negative to swab specimens (PCR) and he has after computed tomography (CT) imaging of her chest a complete resolution of bilateral areas of altered density a ground glass after treatment. Emogasanalysis FiO2 28% pH 7.45, pO2 86 mmHg, pCO2 38 mmHg P/F 307 (Figure 1).
Physiatrist evaluation revealed: global muscular hypotrophy more pronounced in the lower limbs, all active movements present with muscle strength deficit MRC 3/5. In particular, deficit of dorsal flexion of the foot, greater on the left, as a result of previous Guillain-Barré syndrome. Started a program of global motor rehabilitation with global functional rehabilitation and gait training for recovery of motor skills.
Discussion
Comorbidities are associated with severe Sars-Cov-2; while they were recorded in 24% to 51% of hospitalized patients, [5] they were noted in 68% to 72% of ICU patients [6]. The common comorbidities recorded in reports from China (and elsewhere) included hypertension, cardiovascular disease and diabetes mellitus, [7] all of which are known to be associated with obesity and indeed obesity itself is increasingly recognized as both a comorbidity and a risk factor [8].
Sars-Cov-2 in our obese patient caused Severe Interstitial Pneumonia and increased the risk factors and co-morbidities (arterial hypertension, diabetes mellitus type II, previous Guillain- Barré syndrome, obesity III degree with BMI=40). It is extremely important to implement strategies for early diagnosis of these particular patients and to follow them also in the post Covid period.
The chronic inflammation in patients with obesity is speculated to be contributory to the observed increased mortality due to a potential enhancement of the inflammatory response to COVID - 19 infection and induced disturbances in T-cell mediated immunity [9]. Indeed, obesity has been associated with increased activation of pro - inflammatory T - helper (Th -) 1 and Th - 17 cells with reductions in anti?inflammatory Th - 2 and regulatory T-cells [10]. An elegant study by demonstrated that not only were memory T cell quantities increased in obesity, their function was disrupted leading to tissue destruction following viral infections [11]. A more recent study of peripheral blood mononuclear cells showed enhancement in TNF - and Fas - induced T cell- apoptosis in patients with COVID-19 [12]. The T - cell response is increasingly being postulated as being pivotal in reducing susceptibility to and adversity from SARS-CoV-2 and impaired T - cell immunity may be key to obesity?related detriment in relation to COVID-19.
Obesity is characterized by adipose tissue remodeling, and pro - inflammatory alteration of the adipokine profile. The resultant imbalance between pro - and anti?inflammatory adipokines have been implicated as key to obesity being a major risk factor for acute lung injury [13].
Our current understanding of obesity as an independent risk factor for severity of COVID-19 is borne out of observational studies. Further research is necessary to better elucidate the cellular and molecular mechanisms that underlie this increased risk. Urgent research is also required into pharmacotherapeutics for COVID-19 in people with obesity to better understand efficacy and failure of antiviral drugs, immunotherapies and vaccines. Whether significant weight loss in people with obesity, particularly massive weight loss after bariatric surgery, influences outcomes of COVID-19 remains to be seen and needs further study. Ultimately, research into the biological, psychological, socio?cultural and economic drivers of obesity and its management are essential for building societal resilience to future pandemics.
Conclusion
Obesity is a risk factor in viral pandemics and infected patients with obesity have a worse prognosis and Sars-Cov-2 is no exception.. During pandemics individuals with obesity should be included as one of the clinically vulnerable groups, especially those with morbid obesity (BMI > 40 kg/m2). Clinical trials should emphasize the inclusion of people with obesity to better understand the effects of obesity on pharmacokinetics. Further research into vaccination regimes is necessary to achieve and maintain better immune response in patients with obesity to subsequent virus exposure.
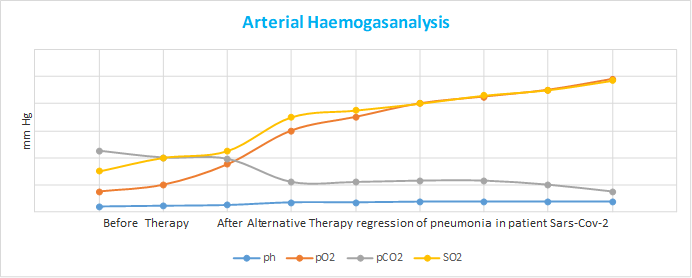
Figure 1: This figure show Arterial Haemogasanalysis before Antiviral Agents, Ventilation and Rehabilitation and After Therapy with Regression of Severe Insterstitial Pneumonia.
Guan W, Liang W, Zhao Y, Liang HR, Chen ZS, et al. (2020) Comor- bidity and its impact on 1590 patients with Covid?19 in China: a na- tionwide analysis. Eur Respir J 55: 2000547.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, et al. (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS?CoV?2 admitted to ICUs of the Lombardy region, Italy. JAMA 323: 1574?1581.
Yang J, Zheng Y, Xi Gou X, Pu k, Chen Z, et al. (2020) Prevalence of comorbidities and its effects in patients infected with SARS?CoV?2: a systematic review and meta?analysis. Int J Infect Dis 94: 91?95.
Sattar N, McInnes IB, McMurray JJV (2020) Obesity a risk factor for severe COVID?19 infection: multiple potential mechanisms. Circula- tion 142: 4-6.
Chiappetta S, Sharma AM, Bottino V, Stier C (2020) COVID?19 and the role of chronic inflammation in patients with obesity. Int J Obes (Lond) 44: 1790?1792.
Zhou H and Liu F (2018) Regulation, communication, and functional roles of adipose tissue?resident CD4+ T cells in the control of meta- bolic homeostasis. Front Immunol 9: 1961.
Misumi I, Starmer J, Uchimura T, Beck MA, Magnuson T, et al. (2019) Obesity expands a distinct population of T cells in adipose tissue and increases vulnerability to infection. Cell Rep 27: 514?524.
Zhu L, Yang P, Zhao Y, et al. (2020) Single?cell sequencing of peripheral blood mononuclear cells reveals distinct immune re- sponse landscapes of COVID?19 and influenza patients. Immunity S1074?7613: 30316?2.
De Oliveira LV and Mafra D (2013) Adipokines in obesity. Clin Chim Acta 419: 87?94.
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras , et al. (2021) High Risk of Severe Sars-Cov-2 in Patient with Obe- sity and Co-morbility: importance of early management from mechanical ventilation to rehabilitation in the Covid-19 Era. Emerg Infect Dis Diag J: EIDDJ-100031. DOI: 10.53634/2652-4449.100031